(NEW YORK) — While the new omicron variant of the COVID-19 virus has not yet been detected in the United States, it will “inevitably” arrive, Dr. Anthony Fauci said Sunday.
“We all know when you have a virus that has already gone to multiple countries, inevitably it will be here,” Fauci told ABC’s This Week anchor George Stephanopoulos. “The question is, will we be prepared for it?”
The omicron variant, named after the 15th letter of the Greek alphabet, was first detected last week in Botswana, officials said. Since then, cases of the new variant have been found in South Africa, Germany, Belgium and Hong Kong.
Pressed by Stephanopoulos on whether the omicron variant is as or more transmissible than the delta variant and other mutations that have swept the globe, Fauci, director of the National Institute of Allergy and Infectious Diseases and the White House chief medical adviser, said, “It appears to be.”
“It has a bunch of mutations,” Fauci said, including “a disturbingly large number of mutations in the spike protein, which is the business end of the virus.”
“Inevitably, it will be here. The question is will we be prepared for it?”
Dr. Anthony Fauci tells @GStephanopoulos that “if and when, and it’s going to be when,” the omicron variant reaches the U.S., health protocols should be “revved up.” https://t.co/cBo22ICrUo pic.twitter.com/AMzK01rlFK
— This Week (@ThisWeekABC) November 28, 2021
Fauci’s comments came one day before the United States plans to impose a travel ban on most travelers from eight southern African countries.
When asked by Stephanopoulos whether the travel ban will make a difference, Fauci said, “It will slow things down.”
“Travel bans, when you have a highly transmissible virus, never completely … prevent it from coming into the country. No way that’s going to happen,” Fauci said. “But what you can do is you can delay it enough to get us better prepared. And that’s the thing that people need to understand.”
He cautioned that traveling during the pandemic is “always risky,” but if Americans have to travel, he recommended they be vaccinated and to wear a mask on flights and in airports, which he described as “one of the most congregate settings you can imagine.”
The chief medical adviser said early signs “strongly suggest” that the variant may be more transmissible and might evade protections from monoclonal antibodies and “perhaps even antibodies that are induced by vaccine.”
Dr. Anthony Fauci tells @GStephanopoulos that the omicron variant of COVID-19 “appears” to be more transmissible than other variants, “might evade some of the protection of monoclonal antibodies and…perhaps even antibodies that are induced by vaccine.” https://t.co/ETIov84eDo pic.twitter.com/gzkaQEHZj6
— This Week (@ThisWeekABC) November 28, 2021
In South Africa, cases of new COVID-19 infections have been heavily weighted toward the omicron variant, Fauci said, so, “you have to presume that it has a good degree of transmissibility advantage.”
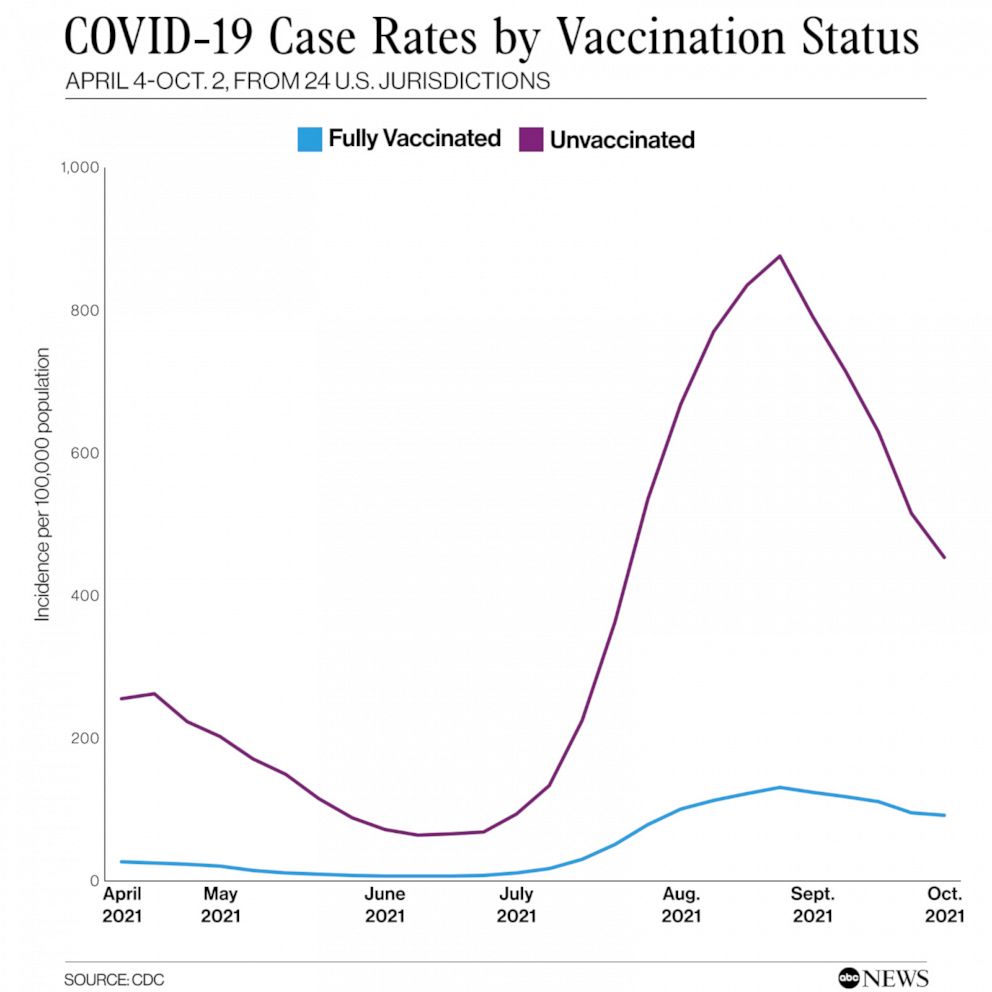
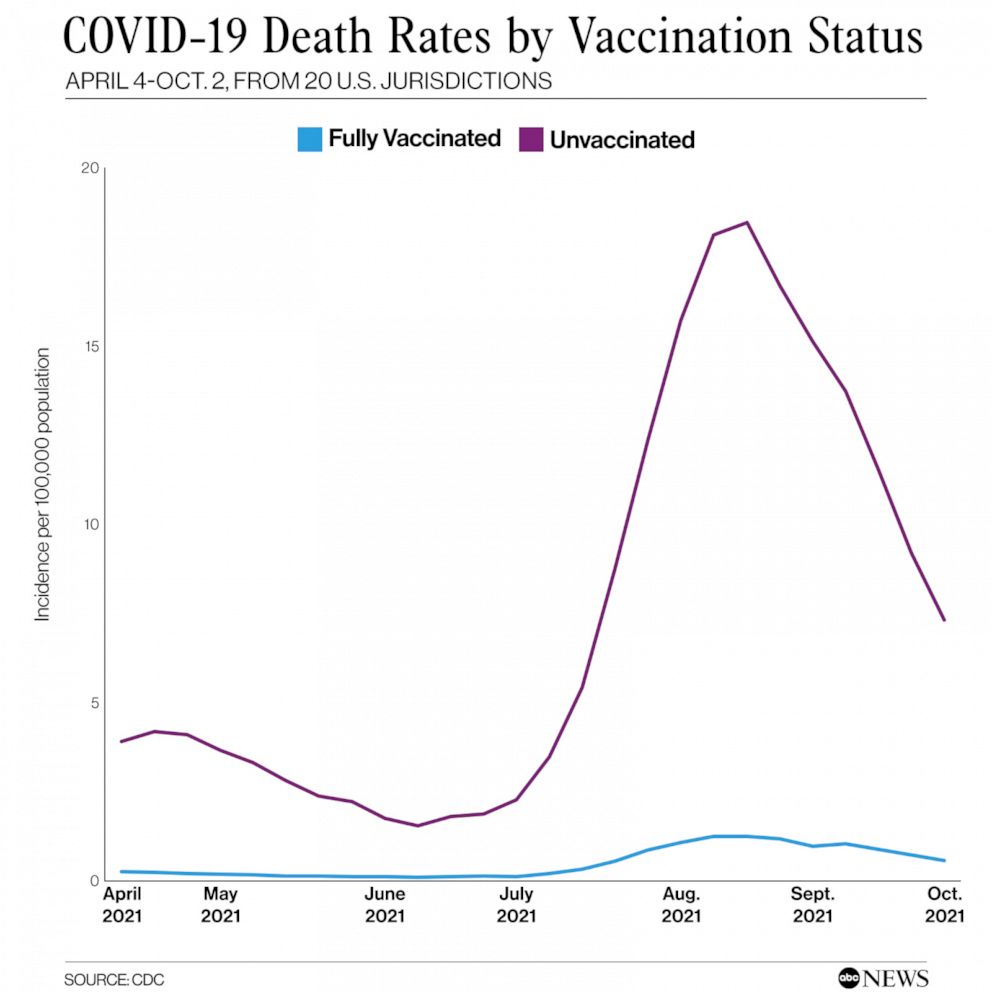
However, Fauci noted that a relatively small proportion of the population of South Africa is vaccinated. According to Johns Hopkins University, just over 24% of people in South Africa is fully vaccinated, compared to 60% of the U.S. population.
“So, you’ve got to take that into the equation when you’re trying to figure out where this virus is really going and what its impact is going to be,” Fauci said.
Asked by Stephanopoulos if omicron causes more severe disease, Fauci said that currently remains a mystery.
He said U.S. scientists spoke to their counterparts in South Africa on Friday and plan to meet with them again later Sunday “to try and find out if the cases they have identified that clearly are caused by this variant, what is the level of severity in that.”
“Hopefully, it will be light,” Fauci said.
Pressed by @GStephanopoulos on whether vaccines can fight omicron variant, Dr. Fauci says “I don’t think there’s any possibility that this could completely evade any protection by vaccine. It may diminish it a bit, but that’s the reason why you boost.” https://t.co/RB4JDN9jsr pic.twitter.com/rE9IxqwtL3
— This Week (@ThisWeekABC) November 28, 2021
Stephanopoulos also pressed Fauci on how susceptible vaccinated people are to the new variant, asking what is known about how resistant omicron is to the currently available vaccines.
Fauci said studies and experiments are already underway to figure out how strong the vaccines are against omicron and estimated it will take about two weeks before scientists get the answers.
“The way you find that out is you get the virus and you put it either as a whole virus or as what we call a pseudovirus, and you take antibodies or serum from people who have been vaccinated, and you determine if those antibodies can neutralize the virus,” Fauci said.
The chief medical adviser said the best way for Americans to prepare for the omicron variant is to be vaccinated, to get a booster shot as soon as they are eligible, and to keep adhering to other protective recommendations such as wearing masks and practicing social distancing.
“We are on the lookout for this. The CDC has a good surveillance system,” Fauci said. “So, if and when — and it is going to be when — it comes here, hopefully, we will be ready for it by enhancing our capabilities via the vaccine, masking, all the things that we do and should be doing.”
Asked for guidance about traveling outside of the country right now, Dr. Anthony Fauci tells @GStephanopoulos that travelers should get vaccinated and “be prudent” about wearing masks in indoor settings like airports. https://t.co/Z7XtvfKbzN pic.twitter.com/QY6dTqclTC
— This Week (@ThisWeekABC) November 28, 2021
When Stephanopoulos broached the possibility of returning to the lockdowns due to the new variant, Fauci said it’s “really too early to say.”
“We just really need to, as I’ve said so often, prepare for the worst,” Fauci said. “It may not be that we’re going to have to go the route that people are saying. We don’t know a lot about this virus. So, we want to prepare as best we can, but it may turn out that this preparation, although important, may not necessarily push us to the next level.”
He added, “Let’s see what the information that we’re getting in real-time tells us, and we’ll make decisions based on the science and the evidence, the way we always do.”
Copyright © 2021, ABC Audio. All rights reserved.